India’s Pivotal Battle Against HIV/AIDS: From Crisis to Global Leadership
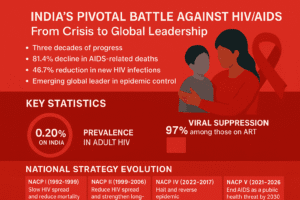
India’s three-decade battle against HIV/AIDS has transformed from a crisis-driven struggle into a global public health success story marked by steep declines in AIDS-related deaths, major expansions in free treatment, and strong progress toward the 95-95-95 global targets. With adult HIV prevalence at just 0.20%—well below the global average—India’s phased National AIDS Control Programme has evolved into a decentralized, rights-based model strengthened by the landmark HIV/AIDS Act of 2017.
Yet regional disparities, especially high-prevalence hotspots in the Northeast, persistent loss to follow-up, HIV–TB co-infection, and challenges for children highlight ongoing vulnerabilities. Sustained community engagement, targeted local strategies, and adoption of next-generation tools like long-acting PrEP will be essential as India strives to end AIDS as a public health threat by 2030 and continues to shape global HIV leadership through affordable medicines and resilient systems.
India’s Pivotal Battle Against HIV/AIDS: From Crisis to Global Leadership
The Turning Tide: A Statistical Milestone
India’s three-decade battle against HIV/AIDS has reached a pivotal moment. While the country still grapples with an estimated 2.5 million people living with HIV, the trajectory of the epidemic has fundamentally shifted. Between 2010 and 2024, India recorded an 81.4% decline in AIDS-related deaths and a 48.7% reduction in new HIV infections. This dramatic progress, propelled by widespread access to free antiretroviral therapy (ART) and robust prevention programs, positions India not only as a national success story but as an emerging global leader in epidemic control.
The numbers tell a compelling story: India’s adult HIV prevalence stands at 0.20%, significantly lower than the global average of 0.7%. The treatment cascade is particularly impressive, with 97% of those on ART achieving viral suppression, a key indicator that the virus is undetectable and untransmissible in these individuals. These achievements are the result of a meticulously planned, evolving national strategy that has transformed India’s approach from crisis management to sustainable public health leadership.
The Evolution of a National Strategy
India’s formal response began in 1992 with the establishment of the National AIDS Control Organisation (NACO) and the launch of its first National AIDS Control Programme (NACP). The program has evolved through five distinct phases, each building on lessons learned and adapting to new epidemiological realities.
The table below outlines the strategic evolution of India’s National AIDS Control Programme (NACP).
| Phase & Period | Core Focus & Strategy | Key Innovations & Outcomes |
| NACP I (1992–1999) | Launch of India’s first comprehensive program to slow HIV spread and reduce mortality. | Established foundational awareness campaigns and safe blood transfusion systems. |
| NACP II (1999–2006) | Reduce HIV spread and strengthen long-term national response capacity. | Began scaling targeted interventions and building institutional frameworks. |
| NACP III (2007–2012) | Goal to halt and reverse the epidemic by 2012. | Introduced District AIDS Prevention and Control Units (DAPCUs) and integrated prevention with care and treatment services. |
| NACP IV (2012–2017) | Accelerate epidemic reversal; aim for 50% reduction in new infections (vs. 2007). | Landmark HIV/AIDS Act (2017), ‘Test and Treat’ policy, Mission Sampark to re-engage patients lost to follow-up. |
| NACP V (2021–2026) | End AIDS as a public health threat by 2030; Central Sector Scheme with ₹15,471.94 crore outlay. | Pursuit of 95-95-95 targets, community-led interventions, and integration with Sustainable Development Goals. |
This phased evolution reflects a shift from a top-down, awareness-driven model to a decentralized, rights-based, and treatment-focused approach. The introduction of the HIV/AIDS (Prevention and Control) Act in 2017 was a watershed moment, legally prohibiting discrimination against people living with HIV (PLHIV) and guaranteeing their right to confidentiality and informed consent. This legal framework, supported by ombudsmen appointed in 34 states and union territories, empowers individuals to seek care without fear.
The Current Landscape: Triumphs and Persistent Challenges
India’s national success masks significant regional disparities. While states like Maharashtra, Andhra Pradesh, and Karnataka continue to bear the largest share of the HIV burden, the most alarming trends have emerged in the Northeast.
- Mizoram and Nagaland now report HIV prevalence above 1%—more than five times the national average.
- Mizoram’s new infection rate is nearly 18 times the national average, driven largely by injecting drug use and changing sexual behaviors.
Despite these hotspots, India’s overall progress toward global 95-95-95 targets—where 95% of PLHIV know their status, 95% of those diagnosed are on treatment, and 95% on treatment are virally suppressed—is strong. According to the latest estimates, India has reached 85% status awareness, 88% treatment coverage, and 97% viral suppression. This places the country firmly on track to meet its 2030 goals.
Key operational achievements include:
- Testing scale-up: Annual HIV tests rose from 4.1 crore in 2020-21 to 6.6 crore in 2024-25.
- Treatment expansion: People on free ART increased from 14.9 lakh to 18.6 lakh in the same period.
- Mother-to-child transmission reduction: A 74.6% decline since 2010 demonstrates the effectiveness of prevention programs for pregnant women.
The Human and Systemic Hurdles
Beneath the positive statistics lie complex human and systemic challenges. Research consistently highlights “loss to follow-up” (LTFU) as a critical weakness. A foundational 2010 study at a major ART center in Delhi found that 22% of patients were lost to follow-up, with most dropping out within the first three months of treatment. This attrition, driven by factors like stigma, economic hardship, and migration, severely undermines program efficacy.
For children, the challenges are even greater. A study on the Early Infant Diagnosis (EID) program found that while three-year survival for infants on ART was a promising 91%, 11.6% were still lost to follow-up and 8.1% had died. Barriers include family-level stigma, desperation about a child’s survival, and logistical hurdles like remote access to pediatric ART centers and lack of child-friendly medicine formulations.
The issue of co-infection, particularly HIV-TB, remains a formidable obstacle. A significant number of TB patients are also living with HIV, complicating treatment and demanding integrated care strategies. As Health Minister JP Nadda noted, poor adherence to treatment regimens requires “intensified counselling, follow-up and community support”.
The Community and Global Context
The heart of India’s response lies in its communities. As Pooja Mishra, a youth coordinator with the National Coalition of People Living with HIV in India, explains, community support is transformative: “The pain, fear, and mental pressure that we ourselves have felt – through that experience – we know how big a role peer support plays in anyone’s life”. Community-based organizations combat stigma, reach vulnerable populations, and provide the essential link between formal healthcare systems and those in need.
Globally, India’s journey holds profound significance. While the international HIV response faces “its most serious setback in decades” due to funding cuts, India has demonstrated the power of sustained domestic investment and political commitment. The country has evolved from a nation struggling with access to expensive medicines to “a net supplier of HIV medicines to the world,” providing affordable, quality generics globally.
The global theme for World AIDS Day 2025, “Overcoming disruption, transforming the AIDS response,” resonates deeply in the Indian context. It underscores the need to build resilient, equitable systems. The World Health Organization’s recent prequalification of lenacapavir (LEN), a highly effective twice-yearly injectable for HIV prevention, represents the next frontier. Integrating such long-acting prevention tools into national programs could be a game-changer for reaching key populations in India and worldwide.
The table below compares India’s current progress with global benchmarks and its own ambitious targets.
| Indicator | India’s Current Achievement (2025 Estimates) | Global 95-95-95 Target | Context & Implication |
| Knowledge of HIV Status | 85% of PLHIV | 95% | Approaching target; indicates successful scale-up of testing campaigns but gaps remain in reaching all populations. |
| On Sustained ART Treatment | 88% of those diagnosed | 95% | Strong linkage to care; the gap highlights challenges like loss to follow-up and access barriers in certain regions. |
| Viral Suppression | 97% of those on ART | 95% | Exceeds target; demonstrates exceptional effectiveness of India’s free ART program and high patient adherence. |
The Path Forward: Ending AIDS by 2030
India stands at a crossroads. The path to ending AIDS as a public health threat by 2030 requires doubling down on what works while innovating to address persistent gaps. This means:
- Hyper-localized Responses: Intensifying focused interventions in high-prevalence states and districts, particularly in the Northeast, with strategies tailored to local drivers like injecting drug use.
- Strengthening the Human Chain: Investing in community health workers, peer educators, and counseling networks to combat stigma and reduce loss to follow-up.
- Leveraging New Technologies: Exploring the integration of new tools like long-acting injectable PrEP (pre-exposure prophylaxis) to prevent infections among high-risk groups.
- Sustaining Rights-Based Approaches: Fully implementing the protective provisions of the HIV/AIDS Act 2017 to ensure a discrimination-free environment for care.
India’s story is one of remarkable public health achievement. It is a testament to the power of combining political will, scientific evidence, community empowerment, and a steadfast commitment to human rights. As the world grapples with disruptions, India’s journey from crisis to control offers a powerful blueprint for resilience, reminding us that even the most daunting epidemics can be overcome with sustained, collective effort.
You must be logged in to post a comment.